This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solveb those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE REPORT
A 58 year old female came to OPD with shortness of breath.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 10 days back then she developed swelling in the legs which is progressive, pitting in nature and gradually progressed up to the knee, accompanied with facial puffiness.
Patient also had burning micturition and decreased urine output. Then she developed shortness of breath 3 days back. Which was persistent even while resting. (GRADE-4)
No h/o chest pain
No h/o palpitations
No h/o abdominal pain
No h/o fever
No h/o cough
PAST HISTORY
Patient was infected with chickengunya 15 years back and went to a private hospital in hyderabad. She started using pain medication for back pain and joint pains from then.
She has been undergoing treatment for chronic renal failure for the last 6 years.
She is a known case of hypertension for last 5 years.
No h/o diabetes
No h/o TB
No h/o epilepsy
No h/o asthma
TREATMENT HISTORY:
Overuse of NSAIDS (pain medications) since 15 years and stopped 5 months ago.
Use of drugs for chronic kidney disease since 6 years.
Use of hypertensive drugs since 5years.
PERSONAL HISTORY:
Appetite: normal
Diet : mixed
Bowel and bladder: burning micturition and decreased urne output ,
normal bowel movements
Addictions : no addictions
Sleep: adequate
FAMILY HISTORY:
None of patient’s parents,siblings,relatives have or have had similar complaints or significant co-morbidities.
GENERAL EXAMINATION:
Patient is consious, coherent and cooperative.
Well oriented to time, place and person.
Moderately built, moderately nourished.
Pallor is present
Pedal edema present (pitting edema)
No icterus, cyanosis, clubbing, generalised lymphadenopathy.
Pulse: Rate: 72 , rhythm (regular), character (normal), volume ( normal)
no radio radial delay
BP: 130/80 mm Hg measured on Right Upper arm in supine position
Respiratory Rate: 25 cpm
RESPIRATORY SYSTEM:
Patient examined in sitting position
Inspection:-
Upper respiratory tract - oral cavity, nose & oropharynx appears normal.
Chest appears Bilaterally symmetrical & elliptical in shape
Respiratory movements appear equal on both sides and its Abdominothoracic type.
Trachea central in position & Nipples are in 4th Intercoastal space
No signs of volume loss
No dilated veins, scars, sinuses, visible pulsations.
Palpation:-
All inspiratory findings confirmed
Trachea central in position
MEASUREMENTS-
AP diameter- 8 inch
Transverse diameter- 12 inches
AP/T ratio - 0.66
Respiratory movement's:- normal on both sides
Tactile vocal fremitus - increased in Infraaxillary & infra scapular area.
Percussion:-
Right left
Supraclavicular- Resonant (R) (R)
Infraclavicular- (R) (R)
Mammary- dull Dull
Axillary- (R) (R)
Infra axillary- Dull Dull
Suprascapular- (R) (R)
Interscapular- (R) (R)
Infrascapular- Dull dull
Auscultation:-
Right Left
Supraclavicular- Normal vesicular NVBS
Breath sounds (NVBS)
Infraclavicular- NVBS NVBS
Mammary- NVBS NVBS
Axillary- NVBS NVBS
Infra axillary- NVBS NVBS
Suprascapular- NVBS NVBS
Interscapular- NVBS NVBS
Infrascapular- NVBS NVBS
PALPATION:
1. No local rise in temperature
2. No tenderness
3. All inspector findings confirmed. (Tracheal position, apex beat)
4. Expansion of the chest: equal in all planes
PERCUSSION:
Resonant all over the chest except mammary and inframammary areas.
PER ABDOMEN:
INSPECTION:
Local rise in temperature.
9 REGIONS
Shape: scaphoid
No Distention of Abdomen
Flanks: full
Umbilicus: normal
The skin over the abdomen: smooth
No engorged veins, visible pulsations, or hernia orifices.
PALPATION: no hepatomegaly no splenomegaly
PERCUSSION:
Normal
No shifting dullness.
AUSCULTATION:
Dull bowel sounds heard.
CVS:
INSPECTION:
Appears normal in shape, apex beat not visible
PALPATION:
All inspectory findings are confirmed.
Trachea is central
No murmurs
AUSCULTATION
S1, S2 heard
INVESTIGATIONS:
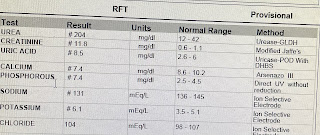
2.12.22
3.12.22
Usg findings:
B/L pleural effusion with underlying lung collapse
4.12.22
PROVISIONAL DIAGNOSIS:
Chronic kidney disease probably due to NSAIDs abuse with severe anaemia and bilateral pleural effusion.
1. Inj. Lasix 40mg IV TID
2.Tab. Nodosis 250mg
3.Tab. Nicardia 10mg
4.Tab. Shellal 500mg
5.Cap. BIOD3
6. Inj. Erythropoeitin 4000IU
Weekly once IV
7.inj. Orofer 100mg IN 100ml
NS IV weekly once


























Comments
Post a Comment