This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
A 64 year old male patient came to casuality with chief complaints of
- unable to talk since 9 days
- bowel and bladder incontinence, loss of appetite , headache since 13days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 12 days back then he developed cough which is insidious in onset gradually progressive which was productive and aggravated on lying down . He developed bowel and bladder incontinence and loss of appetite since 12 days. The patient developed loose stools 5 episodes per day for 1 day which was subsides on medication . He developed having hiccups 8 days back. Since 25/12/2022 he is unable to talk
Fixed flexion deformity
PAST HISTORY
h/o panic attack one month back secondary to family issues
-DM2 since 7 yrs , on medication since 4 years ,
-tab Metformin OD , tab Glimiperide OD
-NO HISTORY OF HTN, Asthma, epilepsy , CAD
PERSONAL HISTORY
Before 7 years he used to work as cattle rearer , after being diagnosed as diabetic he stopped working continuously . He stopped working since 3 years and he uses stick to walk as he is unable to walk properly since 3 years. There is also drastic loss of weight .
Appetite - lost
Diet - Mixed
Sleep - adequate
Bowel and bladder movements - incontinence is present .
Addictions: Occasional alcoholic and tobacco chewing daily .
Allergies : No allergies .
FAMILY HISTORY
There is history of tuberculosis in patients daughter 7 years back and patient's mother 5 years back which was treated.
GENERAL EXAMINATION
Patient is conscious ,incoherent , uncooperative
Moderately Built and Moderately Nourished .
Pallor : present
Icterus : absent
Cyanosis: absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Vitals :-
Temp: Afebrile
BP : 100 / 50 mmHg
PR : 120 bpm
RR : 16 cpm
SPO2 : 98 % at RA
GRBS : 193 mg/dl
SYSTEMIC EXAMINATION:
CNS examination :-
State of consciousness : decreased consciousness
Speech : incoherent
GCS-
E4V1M1
Sensory system :-
Pain - No response
Touch- fine touch - no response
crude touch - no response
Temp - no response
Vibration - no response
Joint position - absent
Cranial nerves : intact
Right Left
Tone :- UL hypo hypo
LL Hypo hypo
Power :- UL and LL not movement even with pain
Reflexes :-
Not elicited
Brain stem reflexes
Conjunctival, corneal, pupillary +
Finger nose in coordination - no
Heel knee in coordination - no
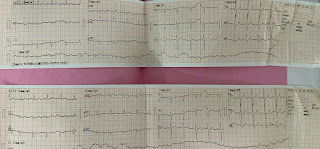
CVS : S1 S2 + ,no murmurs ,no thrills
Respiratory System : decreased air entry on left side . Crepts are heard. Position of trachea - central.
Per abdominal examination:-
Soft , non tender , no signs of organomegaly.
Chest xray
PROVISIONAL DIAGNOSIS
Altered sensorium secondary to meningoencephalitis (? TB )
- Left sided pneumonia ( ?TB )
- prerenal AKI
- bilateral fixed flexion deformity since 2 yrs
TREATMENT
1) IVF 0.9 %NS IV @ 100 ml / hr
2) Nebulization with duolin - 8th hrly , budecort - 12 th hrly
3) Inj .Thiamine 200 mg IV/BD in 100 ml NS
4) Inj . Dexa 6 mg IV / TID
5) ATT therapy PO/OD FDC:3 tab/ day
6) GRBS monitoring 6 th hrly
7) vitals monitoring 6 th hrly
8) Temp monitoring 4 th hrly
9) Inj H. Actrapid insulin SC TID acc to GRBS
10)RT Feeds - 100 ml milk +3-4 scoops protein powder 4 th hrly , 50 ml H2O 2nd
hrly
11 ) physiotherapy was done .
























Comments
Post a Comment